ISPAD 2024: 50 Essential Lessons for Clinicians, Researchers, and Families
The ISPAD 2024 conference, held in Lisbon, was groundbreaking. As the global diabetes community gathered to celebrate 50 years of advancing care for children, adolescents, and young adults with diabetes, the event showcased the latest innovations, research breakthroughs, and clinical strategies aimed at transforming the future of diabetes care. From cutting-edge technologies to new therapeutic approaches, ISPAD 2024 exemplified the power of collaboration across disciplines, uniting researchers, healthcare professionals, advocates, and people living with diabetes (PWD) in the shared mission of improving lives. In this post, I’ve compiled the 50 key highlights that will continue to influence the diabetes landscape for years to come, empowering everyone from patients to policymakers. Each highlight reflects the spirit of innovation and serves as a reminder of the urgent need for access, equity, and collaboration in diabetes care worldwide.
General Highlights for the Public
1. Inclusion & Innovation Theme:
This year’s conference was heavily centered on equity and
inclusivity in pediatric diabetes care. The aim was to highlight disparities
across the globe and foster collaboration to ensure that innovations reach
underserved populations, particularly in low- and middle-income countries
(LMICs). The focus was not just on technology but on ensuring everyone,
regardless of geography or income level, can access these advancements.
2. T1D Screening Programs in Europe:
Italy’s introduction of a nationwide screening program for type 1 diabetes marks a significant milestone in early diagnosis. The general population screening allows for early detection of T1D in at-risk children, which is expected to dramatically reduce rates of diabetic ketoacidosis (DKA)—a life-threatening complication of diabetes that often occurs at the time of diagnosis.
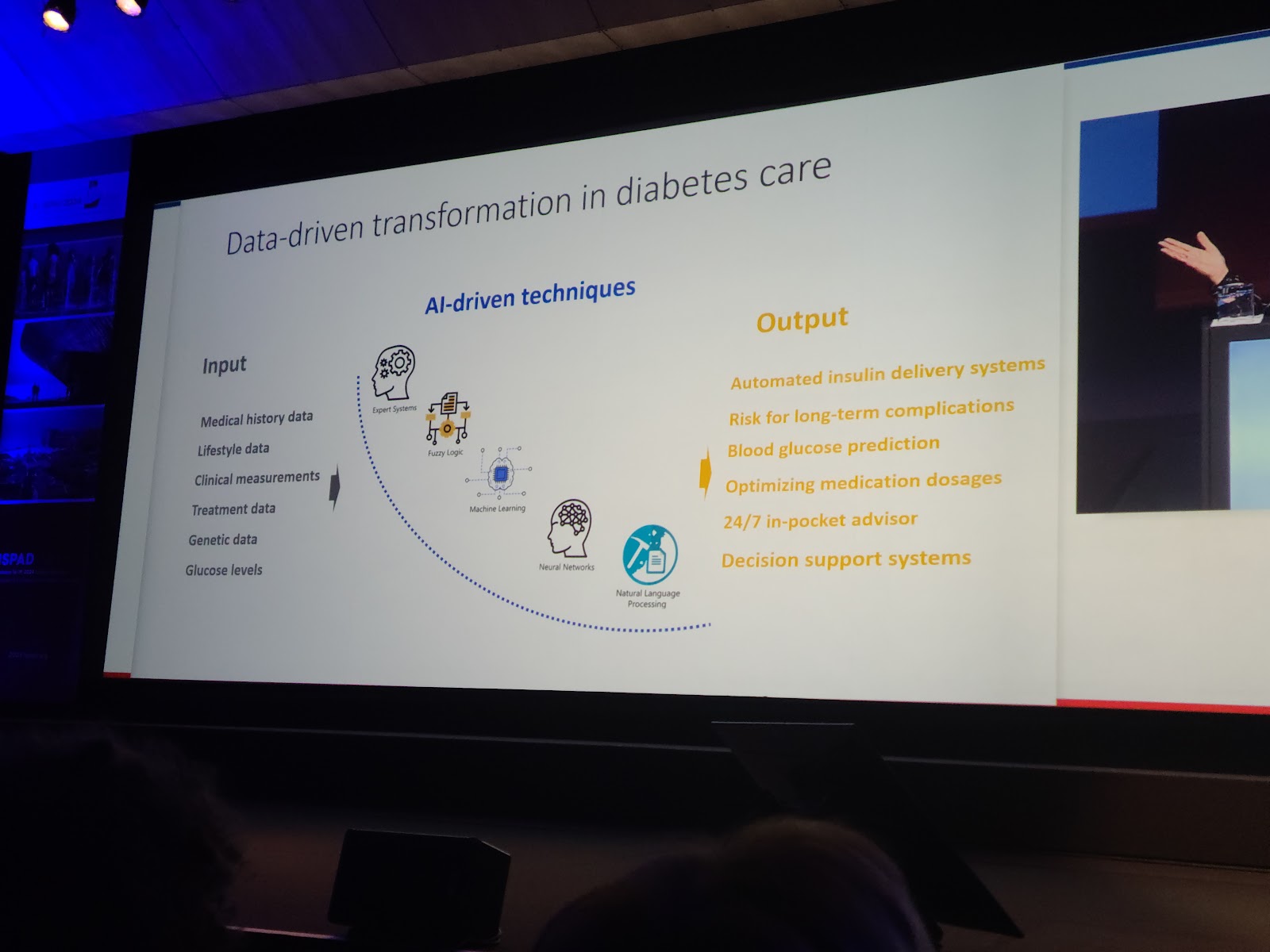
3. Artificial Intelligence (AI) in Diabetes Care:
AI is making a transformative impact on diabetes management, particularly through Decision Support Systems (DSS). These systems can analyze CGMs and insulin pump data, providing tailored recommendations to improve self-management and reduce the risk of hypo- or hyperglycemia. AI also enables more personalized care, improving outcomes for people with diabetes (PWD).
4. Glycemic Management Innovations:
Advancements in CGM technologies, such as longer sensor
life, improved accuracy, and Bluetooth connectivity, are making diabetes
management less invasive and more user-friendly. CGMs are becoming increasingly
integrated with insulin pumps, providing real-time glucose data that allows for
automated insulin delivery. This significantly enhances glucose control for
PWD.
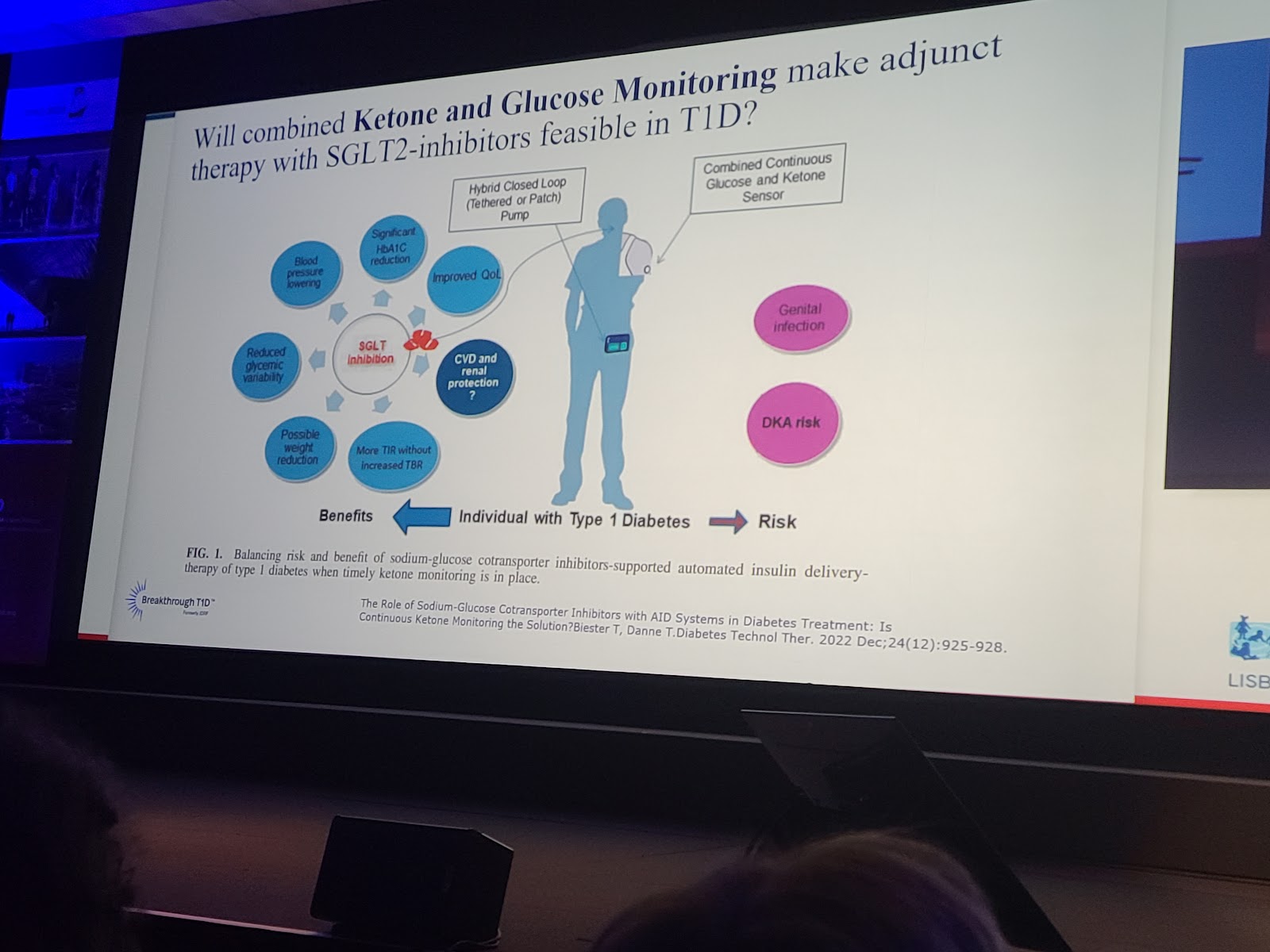
5. Sodium-Glucose Cotransporter Inhibitors (SGLT2):
Research on SGLT2 inhibitors focuses on improving safety and
efficacy, particularly in type 1 diabetes. Combining ketone monitoring with
glucose readings can help prevent diabetic ketoacidosis (DKA) when using SGLT2
inhibitors, making this therapy more accessible and safer for patients.
6. Advancements in Beta Cell Replacement:
Ongoing research in beta-cell replacement therapy is exploring the potential to provide long-term insulin independence for people with T1D. The goal is to restore natural insulin production through islet cell transplants or stem-cell-derived beta cells, offering hope for a functional cure in the future.
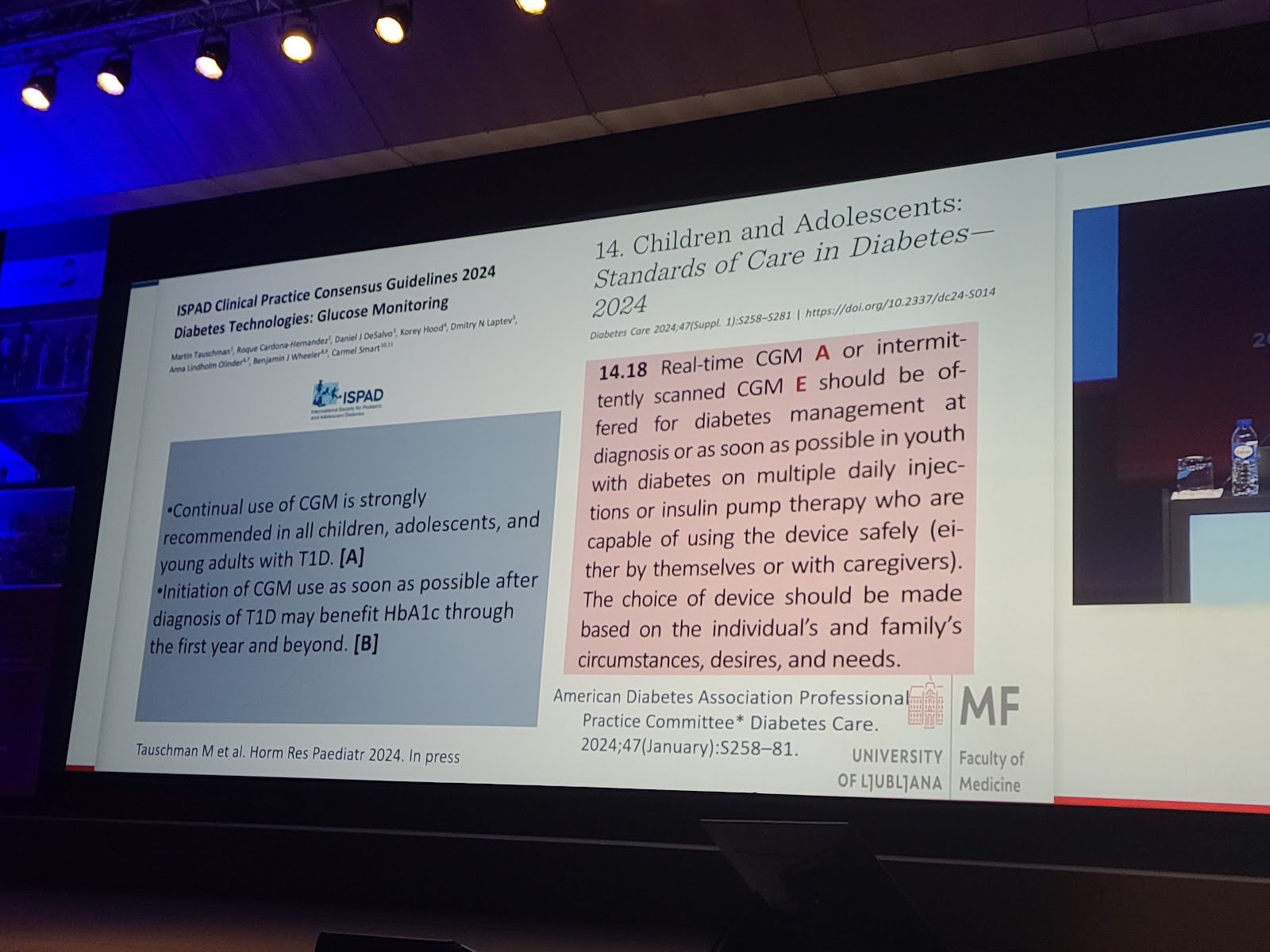
7. Youth-focused Diabetes Care Guidelines:
New guidelines recommend offering continuous glucose
monitoring (CGM) systems to children with diabetes from the time of diagnosis.
Real-time or intermittently scanned CGMs help young patients and their families
manage blood glucose levels more effectively, improving both glycemic control
and quality of life.
8. Psychosocial Support:
The conference emphasized the importance of mental health in
managing diabetes, particularly for children and families. More focus is being
placed on providing psychological and emotional support as part of a
comprehensive care model, recognizing the heavy emotional burden diabetes
management places on families.
9. Capillary Sampling in Youth:
Traditional capillary blood sampling can be uncomfortable,
especially for older children. Researchers are recommending the transition to
dried blood spot (DBS) sampling, which is more stable and less invasive. This
method also allows for easier collection and transport of samples in
resource-limited settings.
10. Global Disparities in Insulin Access:
Despite the progress in diabetes technology, there remain stark disparities in access to basic care, particularly insulin, in lower-income countries. The conference called for increased global cooperation and investment to address these inequalities, as insulin remains unaffordable or unavailable to many PWD worldwide.
For Healthcare Professionals:
11. Holistic Care Approach:
The conference strongly emphasized the importance of a
multidisciplinary approach to treating pediatric diabetes, involving not just
endocrinologists but psychologists, dietitians, social workers, and educators.
This holistic model ensures that both the physical and mental health needs of
young patients are met, leading to better overall outcomes.
12. Diabetes Screening in Early Stages:
A growing body of evidence supports the need for early
screening for islet autoantibodies in children at high risk for type 1 diabetes
(T1D). Early identification could prevent complications like diabetic
ketoacidosis (DKA) and enable healthcare professionals to intervene before the
disease fully manifests.
13. Integration of AI in Clinical Decision-Making:
The integration of Artificial Intelligence (AI) into
diabetes management is helping healthcare providers develop personalized treatment
plans based on large sets of patient data. AI has shown the potential to reduce
clinical workload, improve treatment precision, and tailor diabetes care to
individual needs.
14. Inclusion of Genetic Screening:
Genetic screening is becoming an essential tool in
identifying patients at higher risk of developing T1D. This could allow
healthcare providers to implement preventive measures or more closely monitor
patients who test positive for specific genetic markers.
15. Transition of Care from Pediatrics to Adulthood:
Smooth transition processes are critical as children with
diabetes move into adult care. The conference highlighted the use of new tools
and support systems designed to improve the success of this transition,
ensuring continuity in treatment and reducing the risk of complications.
16. Access to Psychosocial Support:
Increased staffing of psychologists in diabetes centers is
improving the mental health support available to children with diabetes.
Ensuring access to such support can help reduce the psychological burden
associated with managing a chronic condition from a young age.
17. Precision Medicine in Diabetes:
Precision medicine is rapidly becoming a reality in diabetes
care. By using genetic and metabolic markers, healthcare professionals can
customize treatment regimens for individual patients, leading to better control
of blood sugar and reduced long-term complications.
18. Pramlintide in Type 1 Diabetes Management:
Pramlintide, an injectable medication that helps regulate blood glucose, has gained attention as an adjunct therapy for patients with type 1 diabetes. Combined with fast-acting insulin, pramlintide offers a new approach to managing blood sugar, particularly around meals, without the need for excessive insulin doses.
19. Glycemic Control without Carb Counting:
Traditional carb counting can be challenging for patients,
especially children. New approaches, including insulin-and-pramlintide
combinations, are helping patients maintain glycemic control without the need
for meticulous carb counting, reducing the cognitive burden of managing
diabetes.
20. Patient Education on Technologies:
Patient and family education on diabetes technologies, such
as insulin pumps and continuous glucose monitors (CGMs), is crucial for
improving long-term diabetes management. ISPAD stressed the importance of
providing comprehensive training to empower families to take full advantage of
these life-changing technologies.
For Researchers:
21. Immune Modulation in T1D:
Research into immune modulation therapies, which aim to
prevent or delay the autoimmune attack on beta cells, was a major focus. These
therapies hold promise in modifying the course of T1D by targeting its
underlying immune mechanisms, potentially preserving beta-cell function and
slowing disease progression.
22. Clinical Trials in Presymptomatic T1D:
There’s a growing push for more clinical trials focusing on
presymptomatic interventions in T1D. These trials could lead to breakthroughs
in delaying the onset of the disease in high-risk populations and offer
valuable insights into disease prevention strategies.
23. Use of ICD-10 Codes for Presymptomatic Diabetes:
The introduction of specific ICD-10 codes for presymptomatic
diabetes could help standardize care for individuals who test positive for
diabetes-related autoantibodies. This coding system would enable more
consistent follow-up and improve the tracking of disease progression in at-risk
individuals.
24. Beta Cell Replacement Therapies:
Beta-cell replacement through stem-cell-derived or
donor-islet transplants continues to show promise as a potential cure for T1D.
Researchers are making progress in improving the success rates and longevity of
these therapies, though immunosuppression remains a challenge.
25. Data Privacy and AI Implementation:
AI technologies in diabetes management are advancing
rapidly, but issues related to data privacy and security must be addressed.
Researchers are working on new frameworks to ensure that patient data is kept
secure while still enabling the development of AI tools that can enhance
diabetes care.
26. Ketone Monitoring in SGLT2 Inhibitors:
The safety of using SGLT2 inhibitors in patients with T1D is a key area of research. Combining glucose and ketone monitoring may help mitigate the risk of diabetic ketoacidosis (DKA) associated with SGLT2 inhibitors, making this adjunct therapy safer for patients.
Researchers stressed the importance of studying the impact
of educational programs on families dealing with T1D, particularly around the
use of new technologies and early genetic screening. Ongoing research is needed
to determine the best ways to reduce anxiety and improve family support
structures.
T1D has significant psychological impacts, especially when
diagnosed at an early age. Researchers are calling for more studies into the
psychological outcomes of T1D, as well as the development of interventions to
support mental health alongside physical disease management.
29. Long-term Efficacy of Transition Programs:
The effectiveness of programs designed to help young people
transition from pediatric to adult care is still not fully understood. More
longitudinal studies are needed to assess the long-term outcomes of these
transition programs and determine how they can be improved to better support
patients.
30. Capillary Sampling vs. DBS:
Researchers are exploring the potential of dried blood spot
(DBS) sampling as an alternative to traditional capillary sampling,
particularly in children. DBS has the potential to improve the stability of
blood samples during transport and simplify the testing process, especially in
resource-limited settings.
For People Living with Diabetes (PWD):
31. Improved Quality of Life with CGM:
Continuous Glucose Monitors (CGM) have revolutionized diabetes management by providing real-time glucose readings and trends. These devices reduce the need for finger-pricks and allow better glycemic control, which in turn leads to improved quality of life. The ability to monitor glucose fluctuations more accurately helps PWD take proactive steps to avoid hypoglycemia and hyperglycemia, ultimately reducing the risk of complications.
32. Psychosocial Impact of Diabetes:
There’s a growing recognition of the mental and emotional
toll that managing diabetes can have on individuals. The conference discussed
the need for integrating mental health services into diabetes care.
Psychosocial interventions, such as counseling and support groups, are becoming
more widely recommended to help PWD cope with the daily pressures and anxieties
associated with their condition.
33. Access to Innovative Treatments:
New treatments like beta-cell replacement and stem cell
therapies are on the horizon. For PWD, these innovative solutions could provide
a long-term approach to managing or even potentially reversing diabetes. This
exciting development may significantly reduce the need for frequent insulin
injections or pump therapy, bringing hope for more sustainable management of
the disease.
34. AI Tools for Self-Management:
35. Empowerment through Education:
Empowering patients through education was a key theme at the
conference. ISPAD emphasized that well-informed patients are better equipped to
manage their condition. Structured education programs help PWD and their
families understand the complexities of diabetes management, including how to
use new technologies effectively and how to respond to challenges like hypo or
hyperglycemia.
36. Psychological Adjustments to Diagnosis:
Early detection of T1D allows individuals and families time
to come to terms with the diagnosis. Providing psychological support at this
stage can help mitigate feelings of shock, denial, or fear, making it easier to
accept and adapt to the lifestyle changes required for effective diabetes
management.
37. Opportunities in Clinical Trials:
For PWD identified as at-risk through genetic or autoimmune
screening, participating in clinical trials offers an opportunity to access
cutting-edge therapies aimed at delaying or preventing the onset of T1D.
Involvement in these trials provides not only early access to new treatments
but also contributes to the broader scientific understanding of diabetes.
38. Reduced Anxiety Over Time:
Parents and individuals who test negative for islet autoantibodies experience decreased anxiety over time as they become less likely to develop T1D. This provides a level of psychological relief, allowing families to focus on living a more normal life without the constant worry of impending diabetes.
39. Learning Glycemic Management Skills:
For those identified as at-risk but who have not yet
developed full-blown T1D, there is a unique opportunity to build essential
diabetes management skills. Learning how to monitor glucose, adjust diets, and
manage insulin can lead to better outcomes and smoother transitions into more
intensive care if the disease does progress.
40. Fighting DKA with Early Diagnosis:
Early diagnosis of T1D is crucial in reducing the risk of
diabetic ketoacidosis (DKA), a potentially life-threatening complication. By
catching the disease in its early stages, patients can be educated and
monitored closely, greatly reducing the likelihood of DKA, especially in young
children or newly diagnosed individuals.
Other Key Highlights:
41. Telemedicine’s Growing Role in Diabetes Care:
The use of telemedicine has expanded significantly since the
COVID-19 pandemic, offering a lifeline to people with diabetes, particularly
those in remote or underserved areas. Telemedicine enables regular check-ins
with healthcare providers, timely adjustments to treatment plans, and better
disease monitoring—all without the need for frequent in-person visits. This
continues to be an essential tool in managing diabetes worldwide.
42. Supporting Ethnic Minorities:
Ethnic minorities often face unique challenges in diabetes
care, including cultural barriers, socioeconomic disadvantages, and limited
access to healthcare. The conference emphasized the need for culturally
sensitive care models and targeted interventions to reduce health disparities
and improve diabetes outcomes in these populations.
43. Empathy in Diabetes Care:
The conference highlighted that empathy and understanding in
patient-provider relationships are crucial for effective diabetes management.
Healthcare providers who demonstrate empathy can help build trust, which
improves patient engagement and adherence to treatment plans. This
human-centered approach is now seen as integral to improving health outcomes.
44. Parental Anxiety Post-Genetic Screening:
For parents whose children test positive for islet
autoantibodies, the initial diagnosis can lead to heightened anxiety. However,
studies show that this anxiety often decreases over time if the children do not
develop symptoms. Providing counseling and support can help families navigate
this uncertain period.
45. Tailored Diabetes Education Programs:
Educational programs tailored to the specific needs of
families and individuals with diabetes are proving effective. These programs
focus on enhancing self-care abilities, ensuring that both children and adults
are better equipped to manage their condition and make informed decisions about
their health.
46. Challenges with Data Privacy in AI:
While AI offers great potential in diabetes management,
there are ongoing concerns about data privacy and security. As more personal
health data is collected through digital tools, it's essential to establish
robust frameworks to ensure that patient information is protected while still
enabling the benefits of AI.
47. Presymptomatic Education and Counseling:
For families with a genetic predisposition to T1D, early
education and counseling are vital. This helps them prepare emotionally and
practically for the potential onset of the disease. The conference stressed the
importance of providing emotional support during this time, reducing anxiety, and empowering families with knowledge.
48. Expanded Roles for Nurses and Educators:
There’s an increasing call for expanding the roles of
diabetes educators and nurses in patient care. These professionals are critical
in providing ongoing education, support, and care, particularly in settings
where access to endocrinologists may be limited. Their involvement improves
patient outcomes and strengthens diabetes care networks.
49. Family-Centered Care Models:
Family-centered care, where family members are actively
involved in diabetes management, has been shown to improve outcomes for
children with T1D. ISPAD encouraged healthcare providers to adopt this model,
particularly in pediatric care settings, as it leads to better adherence to
treatment plans and overall well-being for young patients.
50. Global Collaboration for Pediatric Diabetes:
The conference underscored the importance of global collaboration in advancing pediatric diabetes care. By sharing research, best practices, and innovations across borders, healthcare providers can work together to reduce disparities in care and improve outcomes for children worldwide.
Conclusion:
The ISPAD 2024 conference has left us with a clear and powerful message: the future of diabetes care depends on the relentless pursuit of innovation, global collaboration, and inclusive solutions. These 50 highlights represent just a fraction of the ongoing work aimed at transforming lives. Now, more than ever, it’s time for healthcare professionals, researchers, and advocates to come together, leveraging collective knowledge to create a future where people living with diabetes everywhere can thrive. As we move forward, let us continue to share insights, champion access to care, and support innovations that bridge gaps, ensuring that no one is left behind. Whether you’re a healthcare provider, researcher, or a person living with diabetes, your voice and actions are essential to building a better tomorrow for all.
Disclaimer:
My attendance at ISPAD 2024 was made possible through the support of both ISPAD and #dedoc°. This post reflects my personal insights and takeaways from the conference.







.png)


thanks for sharing this info
ReplyDeleteEvents like ISPAD 2024 offer invaluable lessons for clinicians and researchers. A Healthcare Management Training Program can help translate such knowledge into practical operational strategies.
ReplyDeleteISPAD 2024 offered vital lessons for clinicians, researchers, and families, demonstrating how knowledge sharing drives innovation. Leaders with a Healthcare Management Executive Program background can translate such insights into actionable strategies, ensuring discoveries move from conferences to clinical practice, improving treatment outcomes, patient education, and long-term approaches to managing chronic conditions like diabetes worldwide.
ReplyDelete