Guiding Young People with Diabetes into Adult Care: #ISPAD2023
,
I was fortunate to attend the International Society for Pediatric and Adolescent Diabetes (ISPAD), ISPAD 49th Annual Conference. The motto of the meeting was “Pediatric diabetes in a rapidly changing world". While research and technology in diabetes develop at astounding speed, the world experiences new problems, conflicts, wars, and economic uncertainties. Especially at such times, working together as ISPAD, securing the best care for children and youth with diabetes remains even more important. Thus, find below my key take-home message from the workshop I attended, entitled ‘Mind the Gap: Guiding Young People with Diabetes into Adult Care’.
Dr. med. Heiko Bratke shared how they helped children transitioning to adulthood at a camp, in Norway. They had individual dose adjustments, group learning sessions, preparing food together (counting carbs and treating acute hypos), and a lot more other things that a young person should manage to become a grownup. Further, the diabetes community has developed its own transition plan, for example, they use streetwise books on different topics relevant to each age group (drugs, sex, rock & roll, school friends, self-management, traveling, and much more). They established annual group meetings with both adolescents and their parents in the hospital (addressing topics like sports & training, traveling, diabetes distress, alcohol, smoking, relationships, sex, pregnancy, driving, and career planning, just to mention but a few). There’s also a camp weekend (once a year) for younger children and for girls from 14 years old and above, they have meetings together with gynecologists. This is believed to detect a lack of transition readiness and develop transition readiness over time. In modern times, they have started sending out digital questionnaires to people from the age of 14, to find out, if there’s a need for further information, education, or other help before they are the adolescents are transferred to adult colleagues from 18yrs.
Here are the hospital results, collected monthly being compared nationally and internationally. Each person with diabetes is tracked individually to find possibilities for improvement.
Dr. med. Heiko Bratke acknowledged the fact that many people are doing a lot of things and they do not have an oversight of what is going on in the world but they just get impressions from clinics that have a special focus on that and it's mostly diabetes-related transition they can read about. Though astoundingly, there is not much about epilepsy or asthma or Crohn’s disease, just to mention but a few.
Sarah Corathers went further to
cover a session on, “The secret of an effective transition into diabetes adult
care. She recognizes that there are lots of contextual variables (geographic,
health system) but she guided the audience to the excellent chapter in the
“ISPAD Clinical Practice Guidelines Pediatric Diabetes 2022”, as shown by the
figure below:
Adulthood is one of the universal
themes (between 18 to 26 years old), where there are many developmental tasks of
gaining autonomy, maybe moving from parental/childhood home, increasing
financial responsibility, maybe exploring intense romantic relationships, and pursuing college. However, all these competing priorities are swelling and
self-management of a chronic condition may not be the top of your priority
list. Dr. Sarah Corathers noted that the aforementioned are some of the contexts and challenges that exist. Hence, she
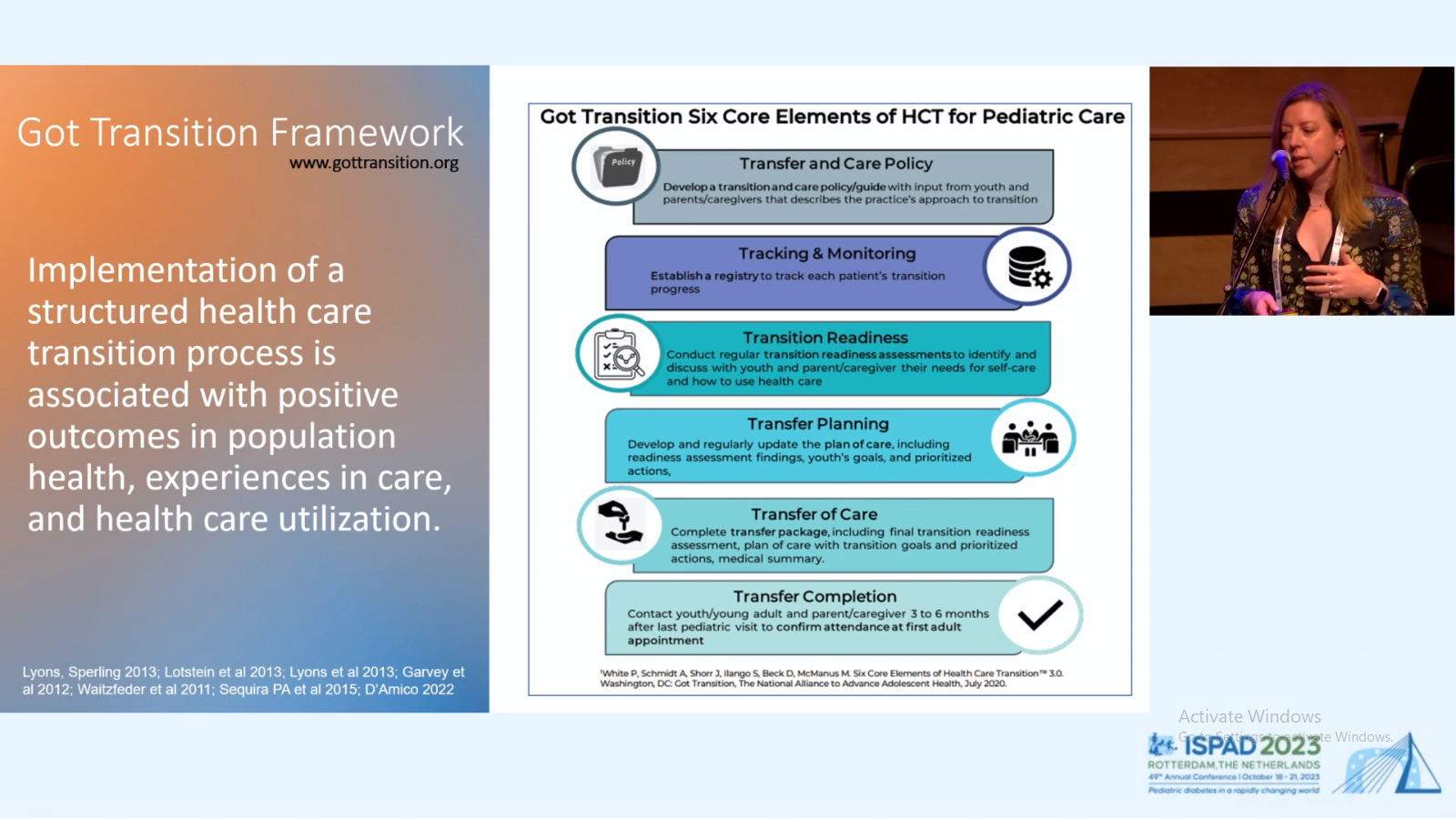
shared about the “Got Transition Framework”, which was thought of as any
pediatric practice that guides youth with a chronic condition, how the
practice might systematically think about preparation, as shown by the figure
below:
Dr. Sarah shared a template, and
she suggested that people who don’t already have one, they should feel free to
modify it, as they need. Below are the Cincinnati
Children’s Diabetes Center Transition Guidelines:
- At diagnosis, patients and families learn that diabetes is a lifelong condition;
- At early adolescence, around age 12, patients should be offered alone time with the physician, nurse practitioner, or education team staff;
- At age 15, the diabetes care team will work with patients and families to develop a transition care plan that can be updated over time.an annual transition readiness assessment will help direct educational interventions;
- At age 18, patients legally become adults. Young adults may provide consent to allow discussion of personal health information with family members;
- All patients, regardless of age are encouraged to involve supportive family, friends and significant others in health care visits and living with diabetes
NB. Transition is not simply from
a health system point of view, but there’s also a series of transitions, as
people emerge through adolescents.
Longitudinal Diabetes Transition Planning:
Healthcare providers, at Cincinnati
Children’s Diabetes Center, have thought about how to operationalize this
transition plan, so that it’s a living, breathing document, in the way that
they deliver care. Here, the providers (the education team members and
transition coordinator), have different roles according to this timeframe.
Transition planning
Diabetes should be a team sport, from a clinical perspective that means that the clinicians, physicians, and nurse practitioners have responsibilities for anticipatory guidance. Adolescents require some time alone with their medical professionals, describing their responsibilities of the adult and the child or teen and then some prompts about anticipatory guidance (some in medical screening & prevention and some in social support, exercise, driving safety, sex etc.). On the other hand, the educational team (which may include social workers), transition plan is are you going to college, are you getting a job, are you moving from the area, do you have a primary care physician, how long do you anticipate staying in pediatric care? All those kinds of details!
Usually, a transition framework doesn’t work if it’s a lopsided model. Thus, if it’s a model with steps for pediatrics but nothing for adult care, then it’s not much of a framework. However, if you do find those adult partners and you want to sort of give them some guidance on where to start, this could be useful.
Further, Dr. Davide Tinti also
delved into this subject matter and he shared the things doctors do not
tell about, from his experience (as a medical doctor) and research. To learn
more about what he shared during this workshop, click
here to watch my summary from his presentation on ‘Mind the Gap: Guiding
Young People with Diabetes into Adult Care’.
Disclosure
In 2023, I was fortunate to have been given access to attend the International Society for Pediatric and Adolescent Diabetes (ISPAD), 49th Annual ISPAD Conference in Rotterdam, the Netherlands, which was held from Wednesday 18 to Saturday 21 October 2023, where I am serving as a voluntary Co-chair for the Membership Committee (which provides me with the same benefits as the elected Advisory Council). Further, #dedoc° provided me with my flights and accommodation, as a #dedocvoice.







.png)


Well written, thank you for all you do sir. Keep doing this beautiful work you do
ReplyDelete