Screening For T1D in Children
Why screening a good
thing?
1.
Primary
Prevention
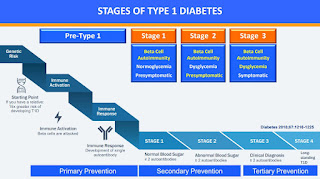
All interventions are intended to hinder the onset of diseases
in the population, fighting the causes and predisposing factors. Often the
intervention aims to change habits and incorrect behaviors (behavioral
intervention)
2.
Secondary
Prevention
Its objective is the early identification of sick or
high-risk subjects in order to achieve healing or prevent the onset and
progression of the disease. Furthermore, a screening test is very important
because it is a medical test or procedure performed on members of a defined
asymptomatic population or population subgroup to assess the likelihood of
their members having a particular disease.
3.
Tertiary
Prevention
It is aimed at reducing the severity and complications of
established diseases
Criteria for
Viability, Effectiveness, and Appropriateness of a Screening Programme
The Condition
1.
The
condition should be an important health problem;
- The incidence of T1D in Children continues to rise by an average of 3-4% per year. In Europe, one out of 250-300 children develops Type 1 Diabetes by the age of 15 years.
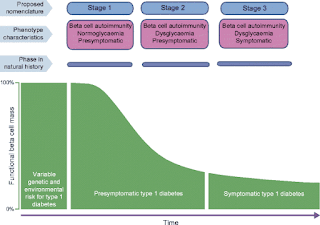
- The epidemiology and natural history of the condition, including development from latent to declared disease, should be adequately understood and there should be a detectable risk factor, disease marker, latent period, or early symptomatic stage
3. If the carriers of a mutation are identified as a result of screening the natural history of people with this status should be understood, including the psychological implications.
Asymptomatic
B-cell Autoimmunity precedes clinical T1D and can be diagnosed by the detection
of multiple islet autoantibodies with a positive predictive value of nearly
90%.
NB. If the child has no risk of autoantibodies, the risk of
developing Type 1 diabetes is similar to the general population
4. There should be evidence from high-quality randomized controlled trials that the screening programme is effective in reducing mortality and morbidity.
The treatment
1. There should be an effective treatment or intervention for patients identified through early detection, with evidence of early treatment, leading to better outcomes than late treatment;
2. There should be agreed evidence-based policies covering which individuals should be offered treatment and the appropriate treatment to be offered;
3. Clinical management of the condition and patient outcomes should be optimized in all healthcare providers prior to participation in a screening programme.
The results
- Teplizumab improves and stabilizes beta cell function in antibody-positive high-risk individuals;
- Teplizumab treatment results in a sustained delay in the diagnosis of T1D during extended follow-up studies;
- Teplizumab treatment increases C-peptide responses;
- Teplizumab treatment reverses declines in C-peptide Area Under Curves (AUC-used to diagnose the Impaired Glucose Tolerance in clinic) during the first 6 months of treatment. This means for people in stage 2, the C-Peptide levels are increased by this drug;
- Teplizumab improves quantitative Oral Glucose Tolerance Test (OGTT- a two-hour test that checks your blood sugar levels before and two-hours after you drink a special drink, that tells how your body processes sugar) glucose area under the curve values.
- For people in stage 2: there was a median delay of Type 1 diabetes diagnosis for about 3 years
- A child diagnosed between 0-10 years loses around 18 years of life because of diabetes.
Targeting regulatory T cells in Type 1 Diabetes Mellitus
Role of IL-2 (interleukin-2) for T-reg cell expansion and safety in children with recent-onset T1DM
- Low-dose IL-2 selectively activates and expands regulatory T cells and thus has the potential to skew the regulatory/effector T cell balance towards improved regulation
- Low dose IL-2 in children is safe at all tested doses!
Benefits of screening
1. Prevention of Diabetic Ketoacidosis (DKA)
It is a life-threatening complication that affects 20-50% of children with new-onset type 1 diabetes in high-income countries. The mortality rate in patients with DKA is less than 1% in children, and DKA is associated with detrimental neurocognitive outcomes and poor long-term glycaemic control.
About DKA…
- Alterations occur most markedly in cerebral white matter, particularly in the frontal lobes, and are most prominent in the youngest children with the most dramatic acidemia (a medical condition marked by an abnormally high concentration of hydrogen ions in a person’s body) during DKA.
- Although changes in Magnetic resonance imaging (MRI) measures over the week after diagnosis resolved, these early brain changes were associated with persisting alterations in attention and memory 6 months later.
Insulin resistance (IR) affects more than half of the adult population
worldwide. Type 2 diabetes (T2D), which often follows, affects more than 450
million people and represents more than 10 % of the health budget in industrialized
countries. A preventive public health policy is therefore urgently needed. Indeed,
early management of IR does not only strongly reduce its evolution towards T2D
but also strongly reduces the appearance of cardiovascular comorbidity as was
suggested by (ATTD Journal, 2019)
ISPAD Clinical Practice Consensus Guidelines 2018: Limited Care Guidance Appendix
The following are the recommended clinical practices for
people living with diabetes, for the prevention of Microvascular and
Macrovascular Complications in Children and Adolescents:
1. Intensive education and treatment should be used in children and adolescents to prevent or delay the onset and progression of vascular complications.
2. Children with type 1 diabetes detected to have positive celiac antibodies on routine screening, should be referred to a pediatric gastroenterologist. If small bowel biopsy is not possible in a child with positive screening tests, then a trial of a gluten-free diet is recommended if celiac disease is suspected. Response should be determined from improvement in growth, bowel habit and reduction in titer of screening antibodies.
3. Screening for complications should be performed preconception and each trimester of pregnancy.
4. Screening for diabetic retinopathy should start from age 11 years with 2 to 5 years diabetes duration and should be performed by an ophthalmologist, optometrist, or a trained experienced observer through dilated pupils via bio-microscopy examination or fundal photography.
5. Blood pressure (BP) should be measured at least annually. angiotensin-converting-enzyme inhibitor (ACEI) are recommended for use in children with diabetes and hypertension, which is defined in children as BP equal to or above the 95th percentile for age, sex, and height, and in Hg. adolescents (age ≥13 years) as systolic blood pressure (SBP) ≥130 and/or diastolic blood pressure (DBP) ≥80 mm Hg.
6. Screening for dyslipidemia should be performed soon after diagnosis (when diabetes stabilized) in all children with type 1 diabetes from age 11.
7. Lifestyle prevention or cessation of smoking will reduce progression of albuminuria and cardiovascular disease.
8. For Type 2 diabetes, complications screening should commence at diagnosis. Attention to risk factors should be escalated because of the increased risk of complications and mortality.
9. Screening for vitamin D deficiency, particularly in high risk groups (eg, darker skin pigmentation, covered clothing, celiac disease) should be considered in young people with type 1 diabetes and treated using appropriate guidelines.
10. Screening for celiac disease should be performed at the time of diabetes diagnosis, and at 2 and 5 years thereafter, as it is frequently asymptomatic. More frequent assessment is indicated if the clinical situation suggests the possibility of celiac disease or the child has a first-degree relative with celiac disease. Screening for IgA deficiency should be performed at diabetes diagnosis.
The #dedoc° voices scholarship program grants diabetes patient advocates free access to the world's most prestigious diabetes conferences: ATTD, EASD, and ISPAD. It provides a dedicated platform for PwD, HCPs, researchers, and industry to meet and exchange: #docday°, #docnight°, our #dedoc° voices networking events, and our exclusive DOClab consultancy sessions. Learn more about it here
Reference:
- Codner E, Acerini CL, Craig ME, Hofer SE, Maahs DM. ISPAD Clinical Practice Consensus Guidelines 2018: Limited Care Guidance Appendix. Pediatr Diabetes. 2018;19(Suppl. 27):328–338. https://doi.org/10. 1111/pedi.12767
- ISPAD 47th Annual Conference (October 13-15, 2021)



.png)


I am thankful to this blog giving unique and helpful knowledge about this topic. excercise for pcos
ReplyDelete